Breast cancer diagnosis
- Turobova Tatiana
- Jan 5, 2017
- 5 min read

The main and additional ways for diagnosis of Breast Cancer (BC) are:
1. breast physical examination (clinical breast examination). This is a careful manual examination of the breasts by a doctor or other health professional. This exam can help find lumps that women may miss with their own self-exams. Lumps, thickening, asymmetry (a difference in appearance between the two breasts) — changes in breasts that a woman may not notice or think are “normal” — may be detected by a health professional who examines many breasts regularly.

2. ultrasonography of breasts. Ultrasound is an imaging test that sends high-frequency sound waves through your breast and converts them into images on a viewing screen. The ultrasound technician places a sound-emitting probe on the breast to conduct the test. There is no radiation involved. Doctors also can use ultrasound to guide biopsy needles precisely to suspicious areas in the breast.


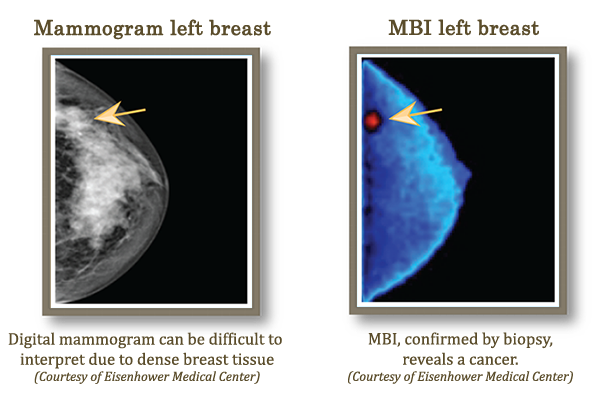
3. mammography. This is the gold standard for detecting BC. Safe and reasonably accurate, a mammogram is an X-ray photograph of the breast. Mammogram may detect microcalcifications, tissue distortion or lumps and may be able to detect the earliest form of BC (pre-invasive) where the cancer hence not able to spread beyond the breast,

Diagnostic mammograms are different from screening mammograms. Diagnostic mammograms focus on getting more information about a specific area (or areas) of concern - usually because of a suspicious screening mammogram or a suspicious lump.

4. ductography for some patients (X-ray examination of a breast with contrast which a doctor inserts to breast's duct via special needle),

5. MRI breasts with contrast injection for some patients (example, women with breast implants ot other previous breast procedures).
Breast magnetic resonance imaging (MRI) uses magnetic fields to create an image of the breast. Breast MRI is more invasive than mammography because a contrast agent is given through or intravenously before the procedure.
MRI does not use X-rays, so it does not involve any radiation exposure.
Breast MRI has a number of different uses for BC, including: screening high-risk women (women known to be at higher than average risk for BC, either because of a strong family history or a gene abnormality) gathering more information about an area of suspicion found on a mammogram or ultrasound monitoring for recurrence after treatment.

6. to confirm diagnosis a doctor can perform a biopsy:
- fine-needle aspiration (FNA) is the least invasive method of biopsy and it usually leaves no scar. the patient is lying down for this procedure. First, an injection of local anesthesia is given to numb the breast. The doctor uses a thin needle with a hollow center to remove a sample of cells from the suspicious area. In most cases, the doctor can feel the lump and guide the needle to the right place. In cases where the lump cannot be felt, the doctor may need to use imaging studies to guide the needle to the right location. This is called ultrasound-guided biopsy when ultrasound is used, or stereotactic needle biopsy when mammogram is used. With ultrasound-guided biopsy, the doctor will watch the needle on the ultrasound monitor to guide it to the area of concern. With stereotactic mammography, mammograms are taken from different angles to pinpoint the location of the breast mass. The doctor then inserts the hollow needle to remove the cell sample.

- core-needle biopsy, This method uses a larger hollow needle than fine needle aspiration does. After numbing the breast with local anesthesia, the doctor uses the hollow needle to remove several cylinder-shaped samples of tissue from the suspicious area. In most cases, the needle is inserted about 3 to 6 times so that the doctor can get enough samples. Usually core needle biopsy does not leave a scar. If the lesion cannot be felt through the skin, the doctor can use an image-guided technique such as ultrasound-guided biopsy or stereotactic needle biopsy. A small metal clip may be inserted into the breast to mark the site of biopsy in case the tissue proves to be cancerous and additional surgery is required. This clip is left inside the breast and is not harmful to the body. If the biopsy leads to more surgery, the clip will be removed at that time.

- excision biopsy. This is the most involved form of biopsy, is surgery to remove the entire area of suspicious tissue from the breast. In addition to removing the suspected cancer, the surgeon generally will remove a small rim of normal tissue around it as well, called a margin. Excisional biopsy is performed with local anesthesia.
- vacuum-assisted breast biopsy (VABB), also known by the brand names Mammotome or MIBB (which stands for Minimally Invasive Breast Biopsy), is a newer way of performing breast biopsy. VABB uses a special probe that only has to be inserted once. The procedure also is able to remove more tissue than core needle biopsy does. For VABB the patient lies face down on an exam table with special round openings in it, where the patient places her breasts. First, an injection of local anesthesia is given to numb the breast. Guided by mammography (stereotactic-guided biopsy) or ultrasound, the surgeon or radiologist places the probe into the suspicious area of the breast. A vacuum then draws the tissue into the probe. A rotating cutting device removes a tissue sample and then carries it through the probe into a collection area. The surgeon or radiologist can then rotate the probe to take another sample from the suspicious lesion. This can be repeated 8 to 10 times so that the entire area of concern is thoroughly sampled.

- radiofrequency (INTAC®) biopsy,
7. Termography also called thermal imaging, uses a special camera to measure the temperature of the skin on the breast’s surface. It is non-invasive test that involves no radiation. Thermography is based on two ideas: due to BC cells are growing and multiplying very fast, blood flow and metabolism are higher in a cancer tumor. As blood flow and metabolism increase, skin temperature goes up. Thermography may be used to supplement information from a mammogram and help identify BC that are close to the skin. Still, thermography can't find cancers that are deeper in the breast and it can't detect small cancers.

8. Molecular breast imaging (MBI) is a new method for detecting breast cancer. The technique is also known as a Miraluma test, sestamibi, scintimammography, or breast specific gamma imaging. MBI uses a radioactive tracer that “lights up” any areas of cancer inside the breast. This tracer is injected into the body through a vein in the arm. BC cells tend to take up the radioactive substance much more than normal cells do. A special camera called a nuclear medicine scanner then scans the breast, looking for any areas where the radioactive substance is concentrated.
8. To exclude or confirm distant metastases doctors can use CT-scan (chest, abdomen, brain), bones' radio-isotopic examination (scintigraphy), PET-scan.
9. Tumor markers (blood tests). A doctor may order blood tests for BC markers to detect cancer activity in the body. A cancer often produces a specific protein in the blood that serves as a marker for the cancer. Protein markers and circulating tumor cells can be measured with simple blood tests. Blood marker tests may be done before treatment, to help diagnose the BC and determine whether it's moved to other parts of the body; during treatment, to assess whether BC is responding; and after treatment, to see if the BC has come back (recurrence). Examples of markers:
- CA 15.3: used to find breast and ovarian cancers
- TRU-QUANT and CA 27.29: may m,
- CEA (carcinoembryonic antigen): this marker may be used to determine if BC has traveled to other areas of the body.

Usually doctors use few kinds of diagnostic procedures for one patient (example, physical examination, ultrasonography and mammography and core-needle biopsy).
At Sen Sok IU hospital for diagnosis of the BC at this moment are available:
1. Physical examination for women with Medical oncologist,
2. Ultrasonography,

3. Mammography,

4. Fine-needle aspiration (biopsy),
5. Excision biopsy,
6. CT-scan,

7. Tumor markers CEA and CA 15.3.



